Laser therapy devices have been used as an adjunct in physical therapy treatments for decades, providing pain relief for injured muscles and joints.1 However, in the past these devices tended to be relatively low in power, requiring extended periods of use to provide therapeutic effects.
Nowadays, more modern devices are capable of delivering therapeutic light energy much faster, but what exactly are the benefits of high power laser treatment?
What is laser therapy?
Laser therapy, or photobiomodulation, applies light energy to the body with the aim of promoting healing. Laser radiation is absorbed in the cell mitochondria and converted into energy (ATP) by the cell, which helps synthesize protein and stimulate the creation of new cells. This leads to the normalization of the affected region by promoting a reduction in swelling, relieving pain, and accelerating the tissue repair process.2
Low level laser therapy devices have an output measured in mW, meaning the time to deliver therapeutic amounts of light energy can make them inefficient, especially when treating deep-lying injuries or large areas such as quadriceps.
High power laser therapy devices, on the other hand, have multiple Watts of power, greatly reducing the treatment times of even large or deep structures. This makes high power laser treatment an effective and practical physical therapy modality.
What are the benefits of high power laser treatment?
From reducing pain to improving mobility, studies have shown there are many documented benefits of high power laser treatment.
Increased hamstring force
In a study by Verma et al. (2022),3 high power laser therapy was used on two groups of athletes with proximal hamstring tendinopathy. The group receiving high power laser therapy in addition to conventional physiotherapy showed an increase in hamstring force (Isokinetic Peak Torque in Nm) of 13% after treatment, compared to 1.5% in the group that received only conventional physiotherapy.
Better shoulder mobility
Atan et al.’s 2021 study4 Involved using high power laser therapy to treat patients with frozen shoulder. Those in the group that received high power laser and exercise showed 60° better shoulder mobility after treatment compared to 38° in the group that used only exercise.
Less tennis elbow pain
A study by Roberts et al. (2013)5 demonstrated that patients who received eight sessions of high power laser treatment experienced a 93% decrease in tennis elbow pain and a 71% improvement of function in the joint. This was compared to no improvement in pain and worsening function in the placebo control group.
Reduced jaw pain
In Ekici’s 2022 study,6 patients with temporomandibular disorder who were treated with high power laser experienced a 55% decrease in jaw pain, compared to 4% of those treated with a placebo laser.
Less carpal tunnel pain
Ezzati et al. (2020)7 showed that patients treated with high power laser therapy benefitted from 68% less carpal tunnel pain compared to 30% with low level laser therapy when using the same fluence (8J/cm.)
Less knee osteoarthritis pain
The knee osteoarthritis patients in Kim et al.’s 2016 study8 experienced 38% more pain relief and 37% additional functional improvement than those who were only given conventional physical therapy.
Less back pain
Patients with lumbar disc protrusion who took part in Chen et al.’s 2018 study9 had 25% more pain relief when high power laser treatment was added to traction therapy than when they received traction therapy alone.
The benefits of LightForce® high power laser therapy
In the field of high power laser treatment, Chattanooga’s® LightForce® laser therapy devices stand out. These products have been used to deliver an estimated 1.2 million treatments per month in 29 countries around the world, enabling clinicians to provide their patients with the beneficial effects of high power laser therapy.
Chatterjee et al.’s 2019 study10 showed that LightForce laser therapy added to standard of care for neuropathic pain resulted in a 30% greater improvement in pain compared to standard of care with placebo laser in patients with diabetic neuropathy.
The same study also demonstrated a 42% greater improvement in quality of life. Furthermore, no side effects or adverse events were reported during the study period, adding to the evidence that high power laser treatment for musculoskeletal disorders is a safe technique.11
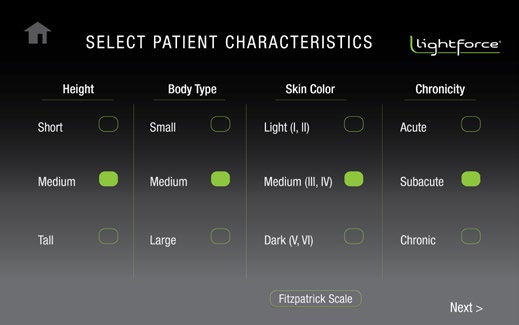
Customers seeking to offer high power laser therapy can choose from three different LightForce devices, each with their own maximum level of power:
LightForce® FXi Therapy Laser – 15W
Portable but powerful
Although lightweight, with a maximum power of 15W, the FXi still has more than enough energy to enable fast, effective laser treatments. Weighing just 3.2kg and with a rechargeable battery that lasts for up to half a day on a single charge, the FXi is a great choice for physios looking to bring the clinic to the patient.
LightForce® XPi Therapy Laser – 25W
The next step in laser therapy
Boasting a maximum power of 25W, the XPi makes treating patients even faster. And with its smart handpiece providing real-time visual and haptic feedback on dosing speed, users can be even more confident in delivering effective high power laser treatment.
LightForce® XLi Therapy Laser – 40W
Maximum power, maximum efficiency
For the busiest practices, the LightForce® XLi provides maximum benefit. With an impressive top power of 40W and the XL Treatment Cone included, clinicians greatly reduce the time needed to treat effectively, allowing them to fit more patients into their daily schedule.
You can download our infographic on the benefits of high power laser therapy here:
To learn more about LightForce therapy lasers visit lightforce.rehab
As laser light can damage the eye, make sure to wear protective glasses during your treatment and never look into the laser beam.
References
- Kitchen, S. S. & Partridge, C. J. (1991). A Review of Low Level Laser Therapy: Part I: Background, Physiological Effects and Hazards. Physiotherapy 77(3): 161-168.
- da Silva, J.P., da Silva, M.A., Almeida, A.P., Lombardi Junior, I., Matos, A.P. (2010). Laser therapy in the tissue repair process: a literature review. Photomed Laser Surg. Feb;28(1): 17-21.
- Verma, S., Esht, V., Chahal, A., Kapoor, G., Sharma, S., Alghadir, A.H., Khan, M., Kashoo, F.Z., Shaphe, M.A. (2022). Effectiveness of High Power Laser Therapy on Pain and Isokinetic Peak Torque in Athletes with Proximal Hamstring Tendinopathy: A Randomized Trial. Biomed Res Int. May 20;2022:4133883.
- Atan, T., Bahar-Ozdemir, Y. (2021). Efficacy of high-intensity laser therapy in patients with adhesive capsulitis: a sham-controlled randomized controlled trial. Lasers Med Sci. Feb;36(1):207-217.
- Roberts, D.B., Kruse, R.J., Stoll, S.F. (2013). The effectiveness of therapeutic class IV (10 W) laser treatment for epicondylitis. Lasers Surg Med. Jul;45(5):311-7.
- Ekici, Ö., Dündar, Ü., Büyükbosna, M. (2022). Effectiveness of high-intensity laser therapy in patients with myogenic temporomandibular joint disorder: A double-blind, placebo-controlled study. J Stomatol Oral Maxillofac Surg. Jun;123(3):e90-e96.
- Ezzati, K., Laakso, E.L., Saberi, A., Yousefzadeh Chabok S., Nasiri, E., Bakhshayesh Eghbali B. (2020). A comparative study of the dose-dependent effects of low level and high intensity photobiomodulation (laser) therapy on pain and electrophysiological parameters in patients with carpal tunnel syndrome. Eur J Phys Rehabil Med. Dec;56(6):733-740.
- Kim, G.J., Choi, J., Lee, S., Jeon, C., Lee, K. (2016). The effects of high intensity laser therapy on pain and function in patients with knee osteoarthritis. J Phys Ther Sci. Nov;28(11):3197-3199.
- Chen, L., Liu, D., Zou, L., Huang, J., Chen, J., Zou, Y., Lai, J., Chen, J., Li, H., Liu, G. (2018). Efficacy of high intensity laser therapy in treatment of patients with lumbar disc protrusion: A randomized controlled trial. J Back Musculoskelet Rehabil. Feb 6;31(1):191-196.
- Chatterjee, P., Srivastava, A.K., Kumar, D.A., Chakrawarty, A., Khan, M.A., Ambashtha, A.K., Kumar, V., De Taboada, L., Dey, A.B. (2019). Effect of deep tissue laser therapy treatment on peripheral neuropathic pain in older adults with type 2 diabetes: a pilot randomized clinical trial. BMC Geriatr. Aug 12;19(1):218.
- Arroyo-Fernández, R., Aceituno-Gómez J, Serrano-Muñoz, D., Avendaño-Coy, J. (2023). High-Intensity Laser Therapy for Musculoskeletal Disorders: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Clin Med. Feb 13;12(4):1479.