As one of the most common health problems, low back pain is a significant problem not just for individuals, but also their families and communities.1 The condition is defined as “activity-limiting low back pain (+/- pain referred into 1 or both lower limbs) that lasts for at least 1 day”.1
As the population ages, the number of people around the world suffering from low back pain is only going to increase.1 Thankfully, back supports such as Lumbostrap 35 and Dorsostrap 55 from DonJoy® can help relieve low back pain.
What are the causes of lower back pain?
There are many potential causes of low back pain:
- Muscle or ligament strain from over-stretching (pulling), heavy lifting, twisting the spine while lifting, vigorous exercise at the gym, or a sudden awkward movement
- Sciatica happens when a weakened and bulging disc is pressed against the sciatic nerve. This can cause intense pain which goes down one leg. This cause can be confirmed through imaging techniques
- Spinal stenosis happens when the space around the spinal cord narrows and puts pressure on the spinal nerves
- Prolonged periods of time incorrectly sitting at your desk (poor posture) can also cause lower back pain
- A herniated disc occurs when an intervertebral disc slides out of position, and spondylolisthesis is when a vertebra slides out of position
Bracing for low back pain relief
A conservative treatment option for low back pain is to wear a back brace. As well as improving postural control,2 the support these devices provide can help to alleviate symptoms associated with low back pain through mechanisms such as activation of the trunk muscles and stabilizing the spine.3,4 They can also help to reduce the use of medication for the condition.5
In patients with low-back pain, walking with abdominal bracing activates the trunk muscles more than walking without an abdominal brace, particularly at slower speeds.3 This means patients incapable of walking faster might possibly benefit from abdominal bracing during walking exercise.3
Patients suffering from low back pain may find that the process of sitting down or standing up can be painful. A study by Im et al. (2021) found that wearing an extensible or a non-extensible lumbar brace has beneficial effects on the biomechanical factors of the sit-to-stand movement in office workers with low back pain.6 It also resulted in immediate reduction of pain intensity and pain-related anxiety.6
Do lumbar braces cause muscle weakness?
One concern about using bracing for low back pain is that it can weaken the trunk muscles. This comes from the assumption that the brace partly replaces the stabilizing function of the trunk muscles.
However, a number of contemporary studies show that back braces do not cause weakness in trunk muscles.7 There is no evidence to the contrary.7
Get low back pain relief with Lumbostrap 35 and Dorsostrap 55 back supports from DonJoy
Lumbostrap 35 and Dorsostrap 55 are two new back supports from DonJoy. These semi-rigid unisex corsets are designed for support and stabilization of the spine and relief of low back pain.
With a height of 35 cm, Lumbostrap 35 provides support and stability for the lumbar spine from S1-T10. At 55 cm high, Dorsostrap 55 covers the dorsal-lumbar spine from S1-T4.
Lumbostrap 35 is anatomically contoured to help provide a comfortable fit and improved patient compliance. Application is made easy through the use of a front closure with a hand loop.
The support’s double bilateral elastic straps are configured in a pulley system, providing independent superior and inferior adjustment of compression level. Conveniently placed within reach, they are easily affixed using hook-and-loop closures.
And four semi-rigid pre-shaped dorsal stays help provide adjustable back support. Two of the stays can be removed and replaced with a more rigid pair for additional stability, and all of them can be reshaped by hand to achieve optimal comfort and fit.
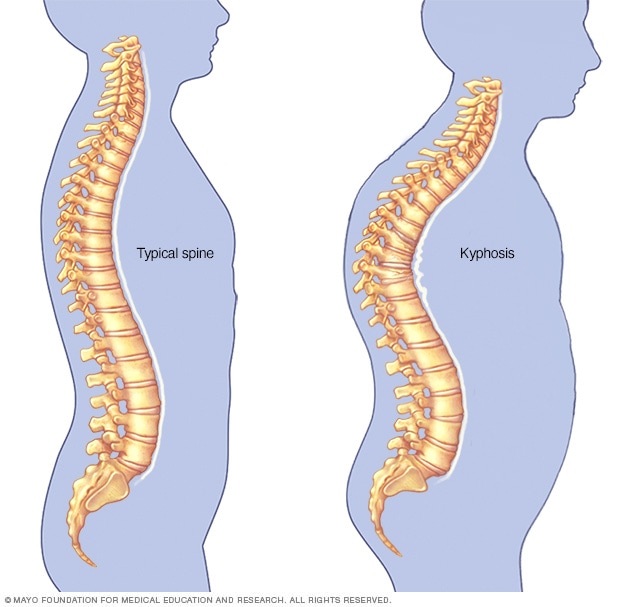
Dorsostrap 55 includes all of the above features, as well as a pair of reverse shoulder straps. Using a traction pulley system, these straps provide adjustable tension to pull the shoulders back and straighten the back, thereby helping to improve kyphotic posture.
Both supports are lightweight, low profile, and breathable, allowing them to be worn comfortably for extended periods, and to fit more easily under clothing. To aid hygiene, they are made from odor-resistant materials which do not include natural rubber latex and are easy to clean.
Intended use and indications
DonJoy Lumbostrap 35 is designed for support and stabilization of the lumbar spine from S1-T10 and relief of low back pain.
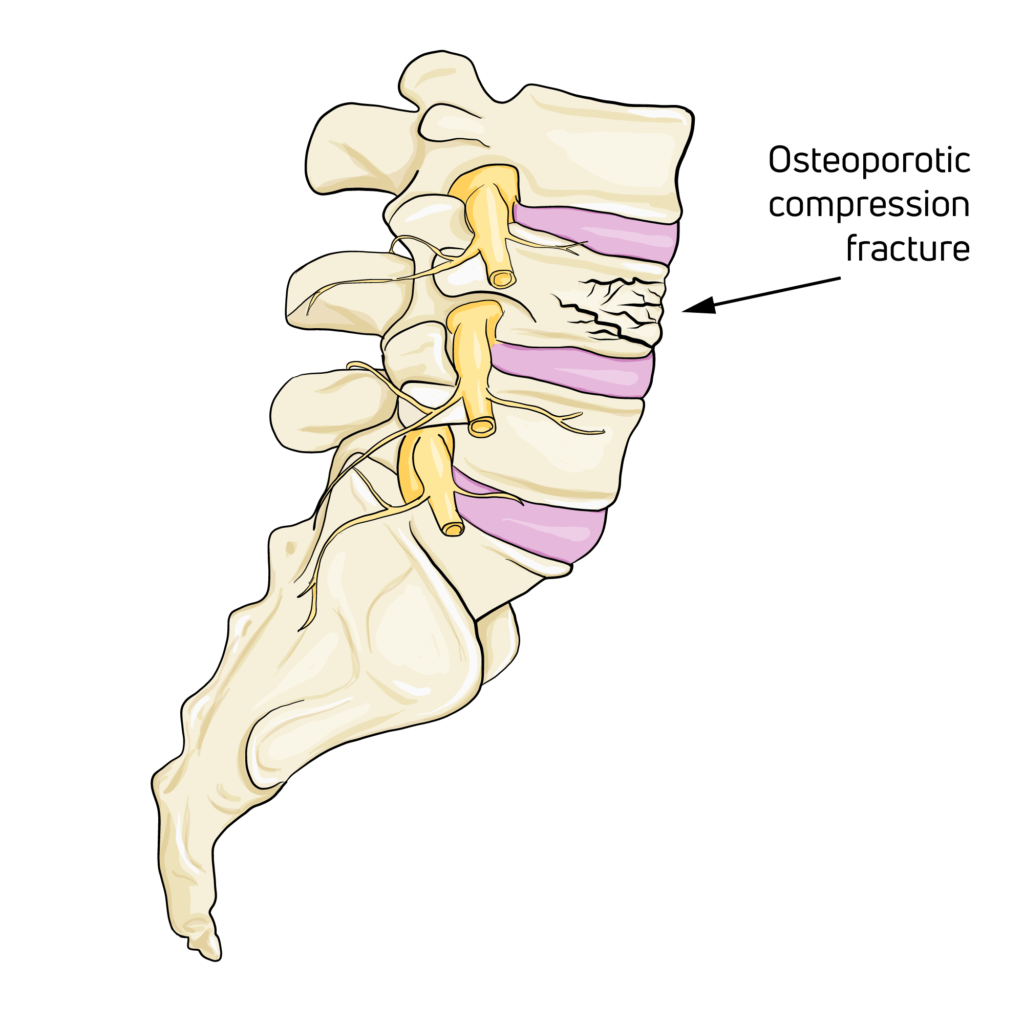
- Results of vertebral collapse (most common indication), that requires a very long usage (up to 12 months)
- Outcomes of vertebral fractures of the lower dorso-lumbar tract
- Post-operation period
- Lumbalgia
- Sciatic lumbalgia and lumbar cruralgia
- Spondylarthrosis and lumbar discopathies
- Slight traumas to the lumbosacral column and paravertebral lumbar contractures
- Treatment of fracture of transverse processes
- Degenerative lumbar scoliosis
- Spondylosis with or without vertebral listhesis
DonJoy Dorsostrap 55 is designed for support and stabilization of the dorsal-lumbar spine from S1-T4 and relief of low back pain.
- Outcomes of vertebral fractures of the dorso-lumbar tract
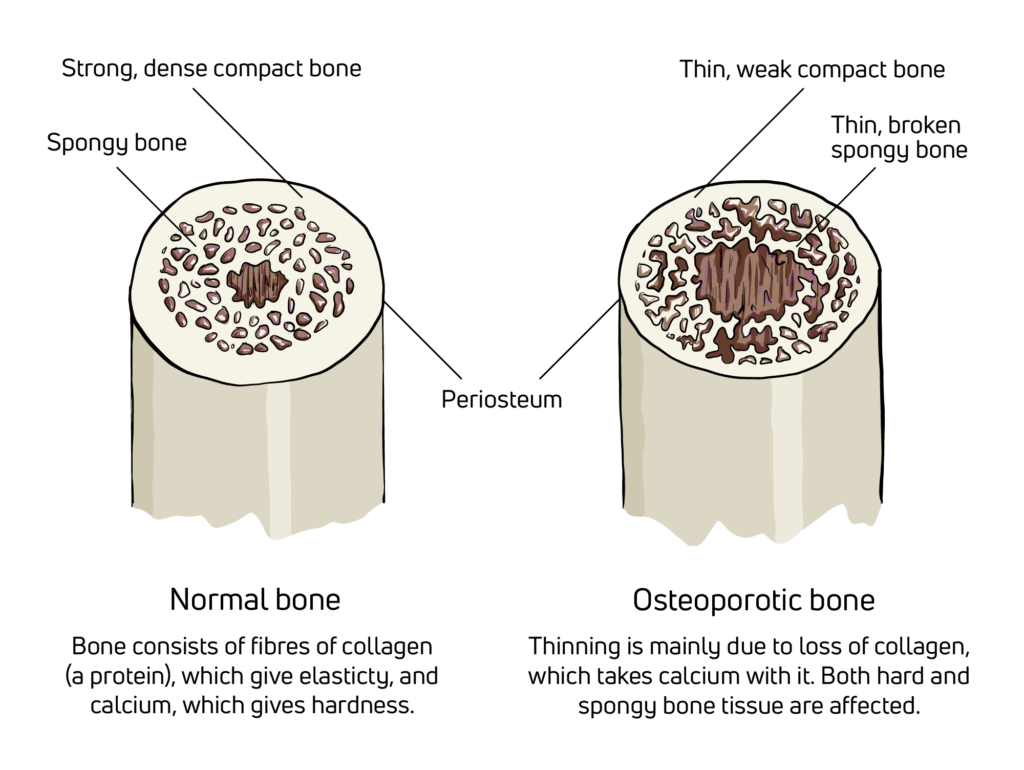
- Dorsal vertebral collapses on an osteoporotic or metastatic basis (most common indication), that requires a very long usage (up to 12 months)
- Post-operation period
- Osteoporosis
- Osteomalacia
- Dorsal kyphosis
- Osteolysis
- Kyphosis with chronic back pain
- Muscular insufficiency
To learn more about these products and others, visit enovis-medtech.eu
References
- Hoy, D., Bain, C., Williams, G., et al. (2012). A systematic review of the global prevalence of low back pain. Arthritis Rheum., 64(6): 2028-2037.
- Mi, J., Ye, J., Zhao, X., Zhao, J. (2018). Effects of lumbosacral orthoses on postural control in individuals with or without non-specific low back pain. Eur Spine J., 27(1): 180-186.
- Soo Choi, J., Kim, H., Lim, J., Seok Ryu, J. (2022). The facilitation of trunk muscles by abdominal bracing during walking in chronic low back pain patients. J Biomech, 143: 111299.
- Ludvig, D., Preuss, R., Larivière, C. (2019). The effect of extensible and non-extensible lumbar belts on trunk muscle activity and lumbar stiffness in subjects with and without low-back pain. Clin Biomech (Bristol, Avon), 67: 45-51.
- Calmels, P., Queneau, P., Hamonet, C., et al. (2009). Effectiveness of a lumbar belt in subacute low back pain: an open, multicentric, and randomized clinical study. Spine (Phila Pa 1976), 34(3): 215-220.
- Im, S.C., Cho, H.Y., Lee, J.H., Kim, K. (2021). Analysis of the Effect of Wearing Extensible and Non-Extensible Lumbar Belts on Biomechanical Factors of the Sit-to-Stand Movement and Pain-Related Psychological Factors Affecting Office Workers with Low Back Pain. Healthcare (Basel), 9(11) :1601. Published 2021 Nov 22.
- Anders, C., Hübner, A. (2019). Influence of elastic lumbar support belts on trunk muscle function in patients with non-specific acute lumbar back pain. PLoS One, 14(1): e0211042. Published 2019 Jan 24.